Differentiating Between the Baby Blues and Postpartum Depression
You did it, moms! You survived pregnancy – the weird discomforts, the strange appendages attempting to bust out of your ever stretching stomach, and that heartburn that just wouldn’t quit. You worked so hard and birthed a beautiful little human who you’ve even kept alive for a few days. And if you’re lucky, you’ve even showered! So you feel great, right? Maybe.
But maybe not.
In a time where moms are told by everyone – from their own mothers to strangers in the grocery store – to “cherish every moment,” many moms are just trying to hang on. The irony and statistical truth is that the majority of mothers will experience some form of mood difficulty in what we are told should be one of the “happiest” times of our lives. Albeit, there is truth in that phrase. Baby blues and Postpartum Depression certainly do not exclude moms from experiencing intense joy, happiness and fun during their first postpartum days, but they can make an inherently challenging and transitional situation all the more difficult.
If we know that the bulk of moms will experience some sort of temporary mood shift during the early postpartum period, the next step is knowing what to watch for. What are the standard symptoms of the baby blues, and how long do they typically last? What’s the difference between the baby blues and Postpartum Depression? Three key factors to consider are duration of symptoms, their severity, and your invaluable intuition as a mom.
Time of Onset and Duration
Due to the massive hormonal shifts immediately following birth, the change in identity as a woman steps into motherhood, the high needs of a newborn, the lack of sleep (and the list could go on!), the majority of women experience some level of heightened emotion within the first few days of giving birth. Baby blues typically begin within a few days after birth and start to wane within one to two weeks. While a mother may continue to experience periods of sadness or worry after that two week window, the feelings will be in proportion to her life circumstances of caring for a newborn.
The timeframe of Postpartum Depression is much broader. Currently, practitioners consider PPD to include the onset of a major depressive episode either during pregnancy or within four weeks after delivery. However, there is a large push within the mental health community to expand that timeframe as the experience of many mothers includes a later onset. For instance, many moms self-report symptoms starting when they transition back to work and leave their baby in someone else’s care, which is typically beyond the four week mark.
Severity of Symptoms
When differentiating between baby blues and PPD, it’s also helpful to consider the severity and pervasiveness of symptoms. Baby blues typically includes symptoms such as tearfulness, sadness, moodiness, irritability, trouble sleeping or eating, and feeling indecisive or overwhelmed. These feelings may be related to expected stressors such as difficulty with breastfeeding, a fussy baby, or lack of sleep. Or they may be triggered by something more unexpected, such as someone else eating the last cupcake. Regardless of what set the baby blues wheels in motion, these symptoms typically do not prevent a mom from caring for herself or her baby. Things may certainly feel more challenging and the symptoms may be present every day, but daily functioning is maintained.
Postpartum Depression, however, carries more severe symptoms that may limit a mom’s ability to manage her daily life. These symptoms can include feeling low or down, a lack of interest or pleasure, changes in eating habits with weight loss or gain, difficulty sleeping or a need for more sleep (beyond what is expected with a baby), feelings of worthlessness, guilt, difficulty concentrating or making decisions, and even recurrent thoughts of death or suicide. Anxiety-based symptoms may also be present, such as feelings of uneasiness, persistent worry and panic attacks. At least some of these symptoms will be present on most days.
When questioning whether you or a friend are dealing with the baby blues or PPD, ask questions such as, “how is this affecting your daily life” and “how is this impacting your ability to care for yourself and your baby?”
Your Intuition
You know who knows you best? YOU. Sadly, many moms receive messages from society to “keep it together” or “suck it up,” as if stepping into the role of motherhood suddenly exempts moms from having needs of their own. While it’s easy to fall into the trap of maximizing baby’s needs while minimizing mom’s, do not allow unfair and unrealistic messages from the world to stifle your intuition that something is off. A gift of motherhood is “the mom gut” – the intuition and sixth sense to know when something is amiss. If you feel like what you are experiencing is beyond the short lived baby blues, you’re probably right. There’s no harm in talking to someone you trust, or seeking help from a professional to check it out.
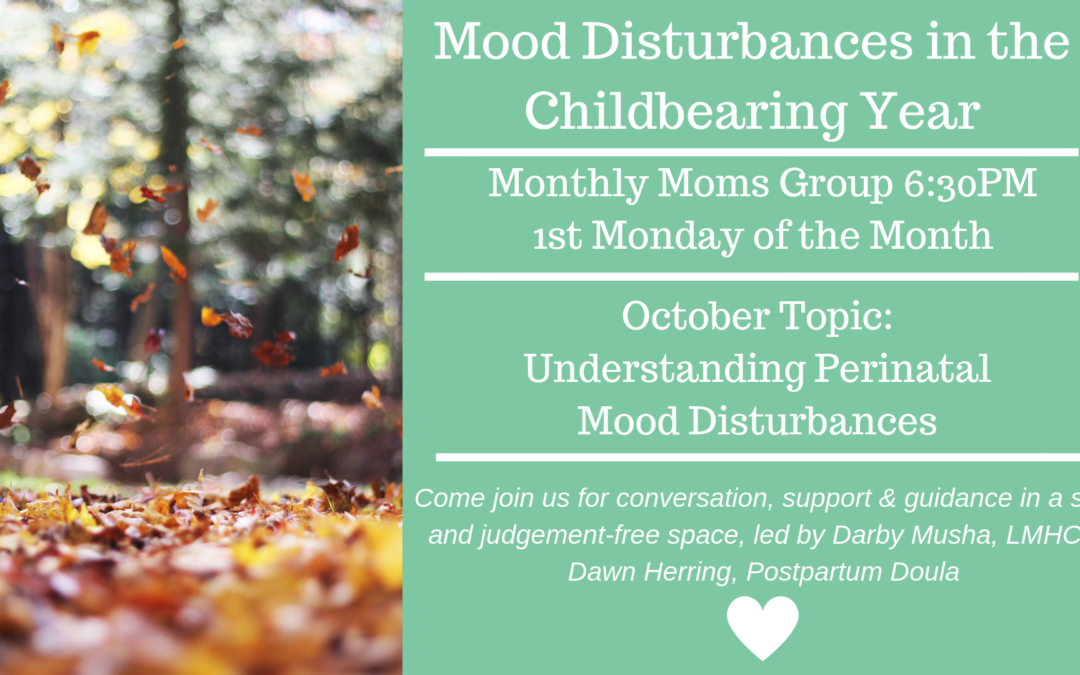
Please join us at Breath of Life on Monday, October 1st to further discuss Postpartum Depression and the baby blues, and how to break the stigma of the diagnosis. This group is for all moms, whether experiencing symptoms past or present, moms wanting to learn more about PPD to support a loved one, or moms simply wanting to connect with others in a confidential, judgment free environment.
Darby Musha is a Licensed Mental Health Counselor providing education and opportunities for moms to process pregnancy and birth-related mental health experiences at Breath of Life.